Conditions
Arrhythmia
Arrhythmia is often suspected when symptoms of palpitation, dizzy spells or syncope are present but can be found incidentally during a routine pulse check by your own doctor. There are several different types of arrhythmia or channelopathies which may cause such symptoms including the following:
- Sinus node dysfunction
- Atrioventricular block
- Supraventricular tachycardia (SVT)
- Ventricular tachycardia (VT)
- Ventricular fibrillation (VF)
- Atrial fibrillation (AF)
- Atrial Flutter
- Atrial tachycardia
- Premature atrial or ventricular ectopics
- Bundle branch block
- Inherited or congenital long QT syndrome
- Brugada syndrome
The specific arrhythmic diagnosis requires confirmation, either by 12-lead ECG or continuous Holter ECG monitoring, followed by specialist evaluation. Patients often require a series of blood tests, an echocardiogram to assess for structural abnormalities of the heart, and sometimes an invasive electrophysiological study.
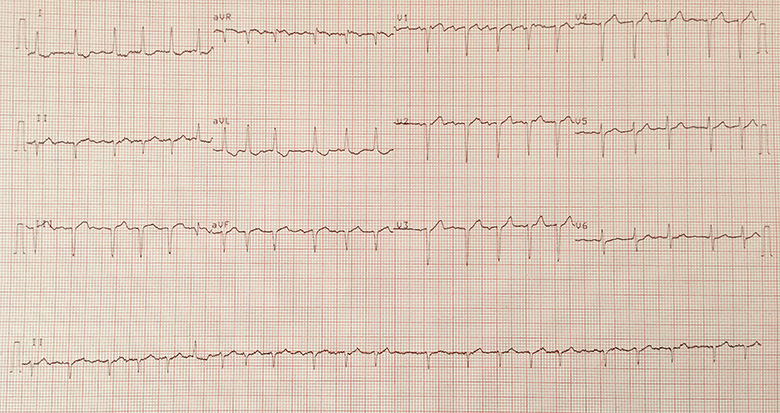
12-lead ECG demonstrating atrial fibrillation
Treatment options will depend on the specific diagnosis. This may consist of simple lifestyle measures alone however certain patients may require prescribed medication including heart rate controlling drugs or anti-arrhythmic drug therapy. Blood thinners called anticoagulants, such as warfarin or direct oral anticoagulants (DOAC), may be required for arrhythmia such as atrial fibrillation in order to reduce stroke risk. Selected patients may benefit from invasive procedures such as electrical cardioversion, catheter ablation procedures or pacemaker/defibrillator insertion.
Angina
Angina is a common cause of chest pain caused by a process called atherosclerosis, leading to narrowing of coronary blood vessels and subsequent reduced blood supply to the heart. This is often called coronary artery disease or ischaemic heart disease. Patients typically describe a heavy, tight or squeezing sensation in the centre or left side of the chest radiating towards the left arm, neck or jaw. Symptoms of angina often occur on exertion but can also develop at rest.
Angina requires urgent assessment, initially with specialist evaluation 12-lead Electrocardiogram (ECG), followed by consideration of non-invasive investigations such as an exercise tolerance test, CT coronary angiogram (CTCA), dobutamine stress echocardiogram (DSE) or nuclear myocardial perfusion scan (MPS).
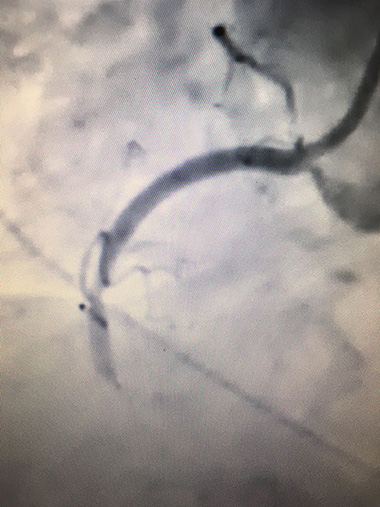
Invasive coronary angiogram showing a blocked right coronary artery
Treatment usually starts with targeting and controlling known cardiac risk factors such as smoking, diabetes, high blood pressure, elevated cholesterol, and achieving lifestyle modification with diet and exercise. Patients with angina often require anti-anginal medication such as beta blockers, an emergency GTN spray, blood thinners such Aspirin, and cholesterol lowering medication such as a statin to control symptoms and reduce the risk of heart attack, known as myocardial infarction. Patients with high risk features may require invasive procedures including coronary angiography sometimes proceeding immediately to angioplasty with stent insertion or referral for cardiac bypass surgery.
Heart failure
Heart failure and cardiomyopathy are forms of heart muscle disease with several potential causes including heart attacks (due to coronary artery disease), valvular heart disease, hypertension, arrhythmia, previous infection of the heart, and can be inherited within families.
Symptoms include breathlessness particularly on exertion, or made worse by lying flat or waking you in the night. Patients may experience fatigue and swelling of the abdomen and legs.
Diagnosis is based on investigations including bloods tests such as natriuretic peptides (NTproBNP or BNP), 12-lead ECG, chest X-ray and Echocardiography. Further assessment is then required to ascertain the precise cause of heart failure which may include coronary angiography, cardiac MRI or a nuclear myocardial perfusion scan (MPS).

Transthoracic echocardiogram- left ventricle and mitral valve
There are many medical treatments available for this condition to both reduce symptoms and hospital admissions but also to improve survival. This usually starts with loop diuretics, ACE inhibitors, beta-blockers, mineralocorticoid antagonists (MRA) and Ivabradine. There are newer drugs available including Sacubitril-Valsartan which may be beneficial in selected patients. Some patients who haven't responded to medical treatment or whom are deemed to be at increased risk of life-threatening ventricular arrhythmia may require invasive procedures such as biventricular pacemaker/defibrillator insertion.
Hypertension
Hypertension, or high blood pressure, is very common but generally a silent condition, unless blood pressure is severely high or long-standing and associated with complications such as stroke, kidney disease or heart failure. A diagnosis of hypertension is made if a consistent resting blood pressure is above 140/90mmHg and should lead to further assessment. The severity of hypertension is based on initial clinic or home readings and often supported by 24-hour ambulatory blood pressure monitor findings.
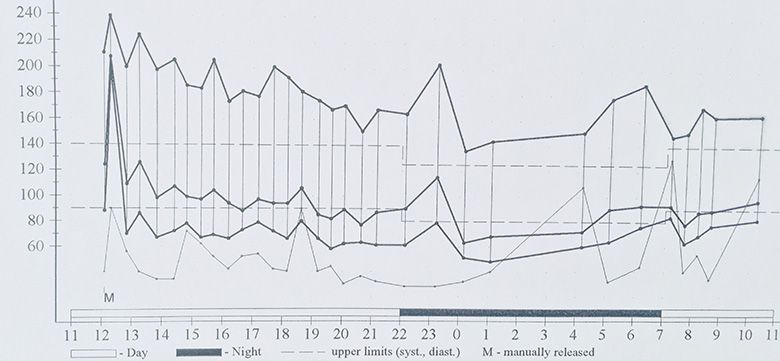
24-hour blood pressure result confirming hypertension
A detailed assessment of cardiovascular risk and any associated organ damage is required. Investigations should include blood tests for renal disease, diabetes and cholesterol, urinary protein levels, 12-lead ECG and Echocardiography. Certain patients will require testing for rarer causes of high blood pressure including metadrenalines for phaeochromocytoma and renin-aldosterone for primary hyperaldosteronism.
Treatment should initially involve strict lifestyle modification including controlled weight loss, stopping smoking, lowering dietary salt, controlling diet and diabetes and taking regular aerobic exercise. Many patients however will require single, or often combination drug therapy, known as anti-hypertensives, to control blood pressure and lower cardiovascular risk.
Hyperlipidaemia
Cholesterol is vital for normal and healthy bodily function however elevated levels of certain types of cholesterol, particularly LDL-cholesterol, is associated with atherosclerosis or narrowing of the arteries within the body. This process can lead to increased risk of angina, myocardial infarction (heart attack) or stroke.
Investigation of cholesterol is by a simple fasting blood test. If elevated, a detailed assessment of your overall 10-year cardiovascular risk and family history are essential to guide management. Certain patients may benefit from further investigation including specialist blood tests, such as LP(a) and apoB, advanced imaging such as carotid ultrasound, coronary calcium scoring or cardiac CT scanning.
Treatment of other cardiovascular risk factors such as hypertension and diabetes are essential. Initial treatment of hyperlipidaemia in low risk individuals may be with simple lifestyle measures including dietary modification, regular aerobic exercise and overall risk factor reduction such as stopping smoking. This is usually followed by re-assessment of lipid profile.
Certain individuals deemed to be high risk will require medical treatment to lower cholesterol with drugs such as statins. Treatment options and doses vary depending on the reason for therapy. If you require statins for prevention of cardiovascular disease, often the lowest required dose is used in order to effectively treat cholesterol levels whilst minimising side effects. High dose statins may required if you have suffered a myocardial infarction irrespective of cholesterol levels.
Valvular heart disease
Valvular heart disease encompasses a narrowing (stenosis), leak (regurgitation), or a combination, affecting one or more of the four heart valves (mitral, tricuspid, aortic or pulmonary). These problems can be congenital, whereby patients are born with the problem, or acquired later in life due to degeneration or infection such as rheumatic fever.
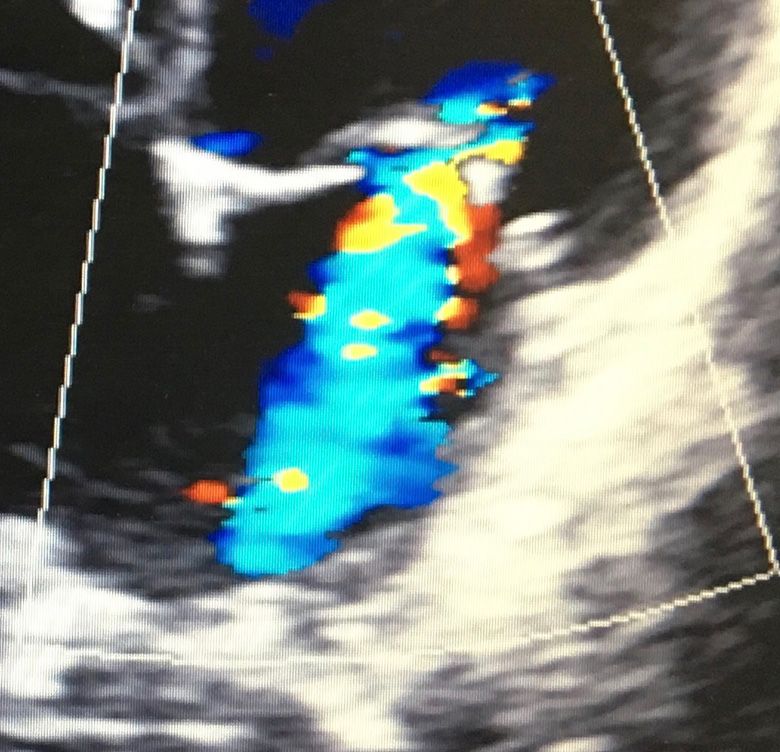
Severe mitral regurgitation
Symptoms can include breathlessness, chest pain, palpitation, fluid overload (oedema), dizzy spells or blackouts. Diagnosis is made by performing an echocardiogram in the first instance. In some patients, further tests such as a transoesophageal echocardiogram, CT or MRI scans may be required.
Treatment of mild or moderate valvular heart disease often includes medication to help alleviate symptoms of breathlessness and oedema whilst aiming to control aggravating factors such as high blood pressure and elevated heart rates, particularly in patients with associated arrhythmia.
Severe valvular heart disease requires urgent assessment for surgical valve replacement to determine potential risks and chance of benefit, the optimal choice of heart valve (metal versus tissue) and need for blood thinners called Warfarin. Surgical treatment requires an open heart operation under general anaesthetic and, on average, a week in hospital followed by a 2-month recovery period. If patients are deemed too high risk for open heart surgery, a less invasive approach such as Transcatheter Aortic Valve Intervention (TAVI) for severe aortic valve disease, could be considered.
Syncope
Syncope, or blackouts, has many potential underlying causes. The clinical history is crucial in understanding the mechanism of collapse and when advising treatment options. Episodes of syncope may be associated with prior dizzy spells, light-headedness, palpitation or frequent falls and should undergo detailed specialist assessment.
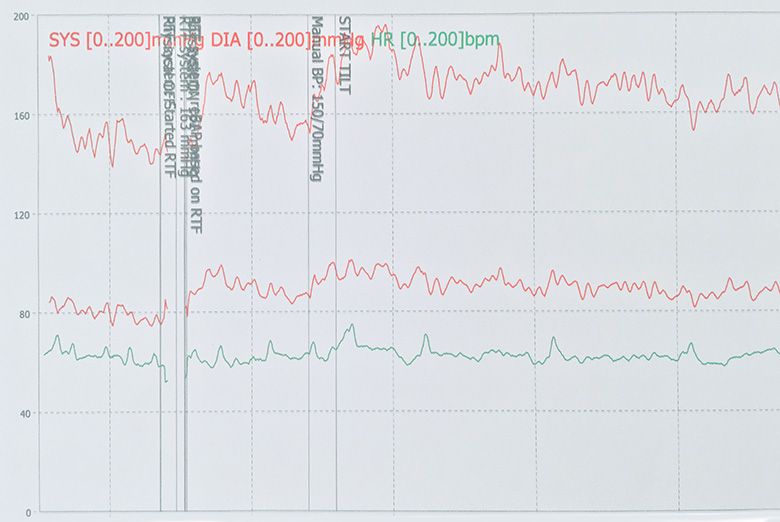
Tilt table test
Investigation of syncope usually entails blood tests, a 12-lead Electrocardiogram (ECG), Echocardiogram, prolonged ECG holter monitoring and certain patients may require a tilt-table test. Insertion of an implantable ECG loop recorder, a day case procedure performed under local anaesthetic, is available for patients suspected to have an underlying arrhythmic cause for syncope.
Management of syncope is dependent on the underlying cause and severity of the condition. Vasovagal syncope, or 'simple' fainting, for example is a common cause and may be triggered by several factors including warm environments, dehydration and emotional stimuli. Postural orthostatic hypotension describes a significant fall in blood pressure on standing and can also cause syncope. These two forms of fainting may be manageable by simple lifestyle modification, patient response to warning symptoms and adjustment to existing prescribed medication. Some patients however may require specific additional medication such as Fludrocortisone or Midodrine to increase blood pressure in order to improve symptoms.
Syncope can also be caused by specific cardiac conditions that require prompt investigation and treatment including arrhythmia, cardiomyopathy or severe heart valve disease. A concerning cause for syncope is bradyarrhythmia (abnormal slow heart rate), such as sinoatrial node disease or complete heart block. In these situations, a permanent pacemaker procedure could be recommended and may be required on an emergency basis.
If syncope is felt to be life threatening, such as hypertrophic cardiomyopathy with ventricular arrhythmia, insertion of an implantable cardioverter-defibrillator may need to considered. An underlying cause of severe valvular disease, such as aortic stenosis, may require urgent consideration of heart valve replacement.

